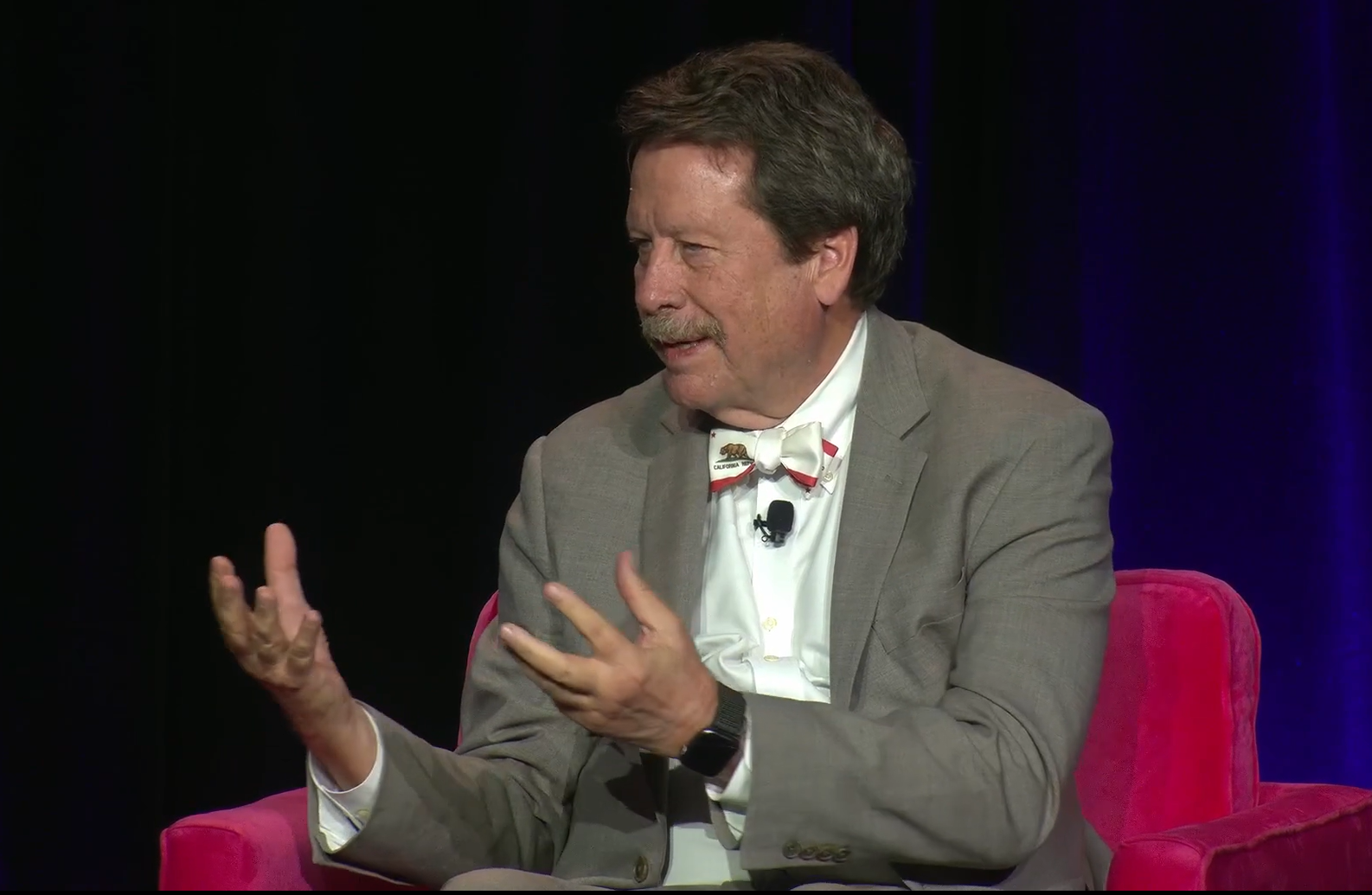
At the HLTH conference held in Las Vegas, FDA Commissioner Robert Califf engaged in a conversation with John Brownstein, Chief Innovation Officer at Boston Children’s Hospital. The discussion focused primarily on the burgeoning sector of healthcare AI and the FDA’s regulatory responsibilities. Califf highlighted the exponential growth within the field and acknowledged the necessity of balancing innovation with regulatory oversight to safeguard public health and improve patient outcomes.
Califf emphasized that the FDA operates more as a referee rather than a constant overseer within the industries it regulates. He clarified a common misconception that the FDA is perpetually regulating; instead, they provide frameworks through laws, rules, and guidances while expecting the industry to self-regulate effectively. This practice is particularly pertinent in the realm of healthcare AI, where stakeholders such as health systems, AI developers, and healthcare data companies play crucial roles in maintaining the integrity of AI algorithms throughout their life cycles. Califf admitted that if the FDA were to monitor everything directly, it would need to expand significantly, which is currently impractical.
One of the major challenges Califf noted was the ongoing validation of AI models in healthcare. He introduced the concept of “local, recurrent validation,” which entails regularly confirming that AI systems perform as expected within their real-world applications. Unfortunately, Califf acknowledged a gap, as he isn’t aware of any U.S. health system currently capable of conducting such thorough validations. He attributed part of this issue to the broader problem of data blocking in healthcare, which impedes the tracking of patient health across different care settings due to inadequate data interoperability.
Beyond operational challenges, Califf also touched on the impact of AI on social equity within healthcare. He expressed concern that AI applications are often used by health systems to segregate patients based on profitability, thereby exacerbating health disparities rather than mitigating them. He emphasized the potential of AI to significantly uplift underprivileged groups if there were a concerted effort to target these populations.
Califf also criticized the state of primary care in the U.S., labeling it as a “disaster” and contrasting the poor health status of Americans with that of citizens from other high-income countries. He lamented the focus on more glamorous technological applications at the expense of fundamental healthcare needs like vaccination and blood pressure control. Drawing a comparison, Califf highlighted Costa Rica’s success in extending life expectancy through a robust network of primary care clinics, suggesting that similar advancements could be achieved in the U.S. with appropriate technological interventions targeting basic healthcare services.
In summary, Califf’s dialogue at the HLTH conference painted a picture of a healthcare landscape at a crossroads, with AI technology offering remarkable potentials for innovation but also posing significant regulatory and ethical challenges. The FDA’s role as a facilitator of beneficial innovation while protecting public health remains a delicate balance in navigating the rapidly evolving healthcare technology environment.
#Worry #FDA #Commissioner #Robert #Califf